
UUtilization ManagementCORE
A member-centric view contributes to Utilization Management outcomes that address the whole person’s care.
Improves outcomes for patients, streamlines entry for providers, and equips clinicians with a 360-degree view of the member.

Features and Functionality
- Pharmacy / medical authorization
- Integration with pharmacy databases
- Track cost savings
- Network integration
- Member 360 view
- Track authorization history
- Provider portal
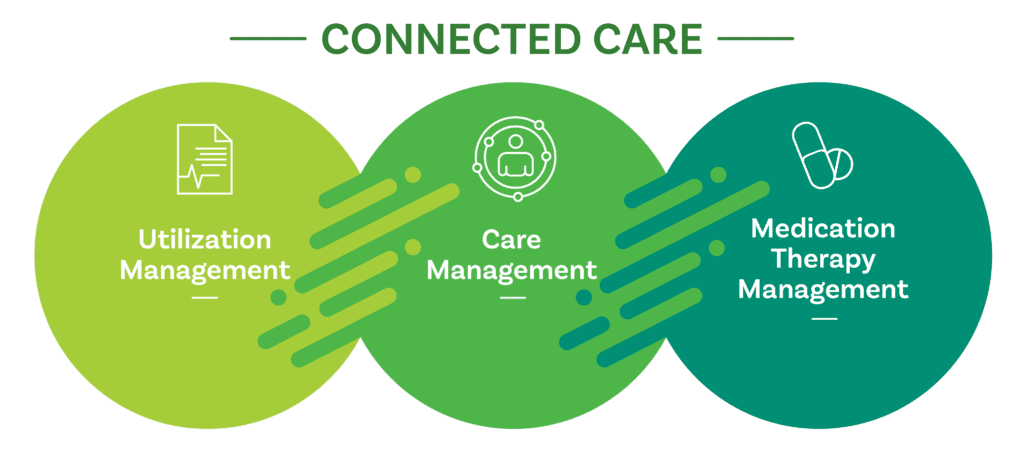
Combine these modules for even greater benefits.
Who We Serve
Learn













